by Ashley Bennett, Director of Trauma-Informed Care
For instance, I wear sunglasses all the time-sometimes even indoors and with certain lighting, and always outside even on a cloudy day. When I put sunglasses on and it dims the light, I immediately feel better. We have an overhead light in our dining room and a lamp-my kids always put the light on, and I always come behind them and turn it off and turn the lamp on. The majority of lights in our house are almost always off. I obviously have a sensory preference for dimly lit spaces.
Most of us have sensory preferences but we can move through our days relatively easily, and our sensory needs don’t interfere with our daily functioning. But for some of us, we are greatly affected by our senses, and we may even have something referred to as Sensory Processing Disorder—which means that the way we are taking in information from our senses is interfering in our daily functioning at home or at work or at school.
Now we could spend an entire module talking about sensory needs but we don’t have time to do that here, so I’ll just say this: due to in-utero drug and alcohol use and/or years of neglect—your children are more likely to have sensory needs that interfere with their daily functioning than their peers. This means that they take in sensory information from the world around them in the same way but that when it reaches their nervous system, it’s interpreted differently. They may avoid certain sensory experiences (like reacting negatively to loud sounds, disliking certain fabrics of clothing, or pushing away from tight hugs) or they may crave certain sensory experiences (like really enjoying spicy foods, seeming to never tire of swinging back and forth on a swing, or can be found hanging upside down on the couch while watching tv).
The two ways we see this play out the most for our kids is in the two senses that are referred to as internal senses-that is proprioception (body sense-having to do with deep muscle pressure) and vestibular (movement sense-having to do with balance). Your child might have a proprioception need if they seem to crave tight pressure, prefer tight hugs, enjoy weighted blankets, and enjoy wrestling and roughhouse play, etc. Your child might have a vestibular sensory need if they tend to hang upside down a lot, twirl, spin, are constantly moving, or appear hyperactive.
If you think that your child might have a sensory need of any kind that is interfering in their daily success, then you’ll want to have them evaluated by an Occupational Therapist (OT). If your child is under the age of 3, you can call Early Intervention for this service. If your child is over age 3, you’ll want to look at your school for resources and/or find a local clinic that does OT evaluations. If your child is on Medicaid, you should be able to access this evaluation for free. I have seen OT services be very beneficial to many of our children.
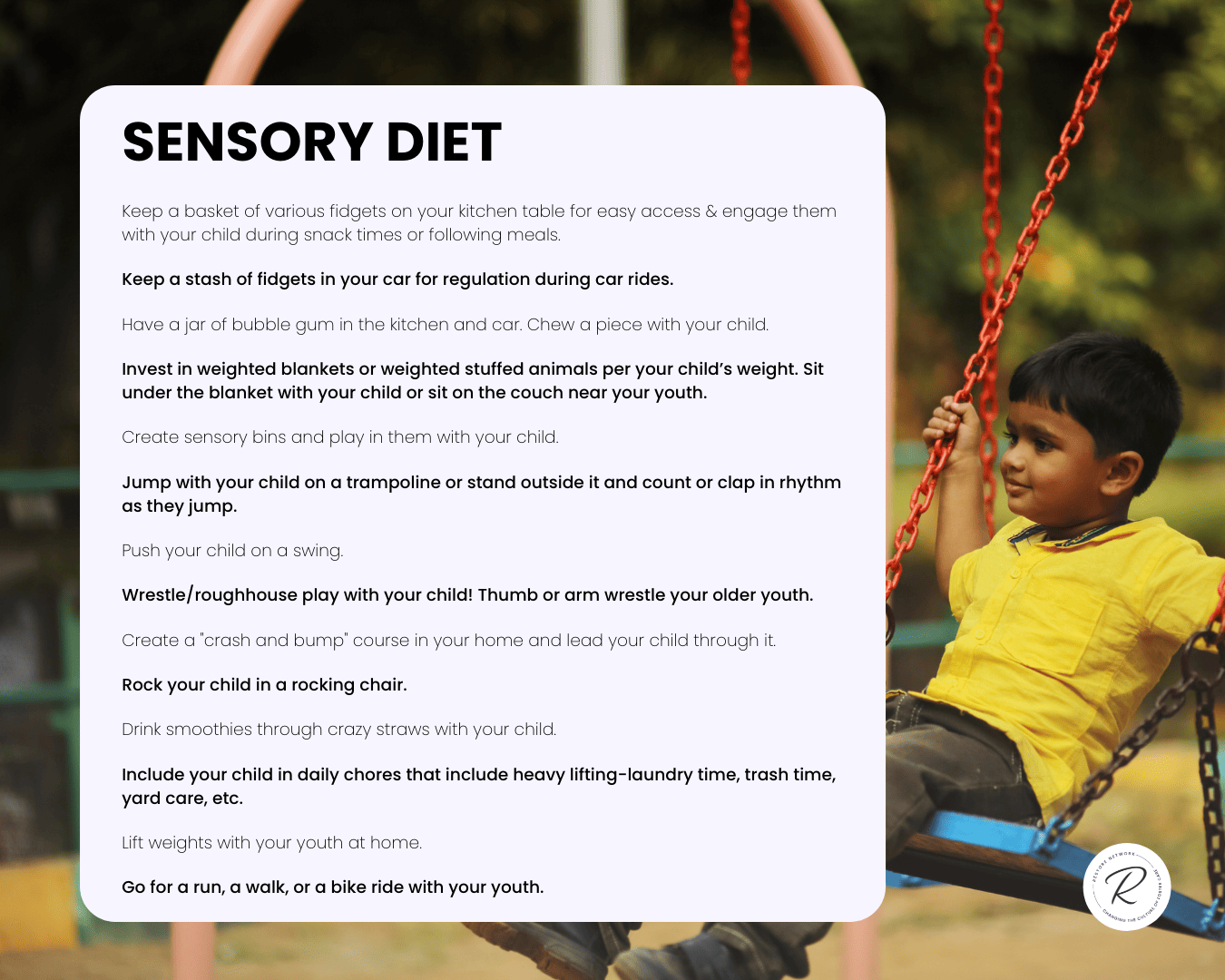
Even if you don’t think your child has a sensory need that is affecting their life, it’s good to just note what your child is drawn towards or moves away from so you can help learn about the tools that can help your child to regulate. For instance, maybe as part of his sensory diet, your child needs to curl up for 30 minutes after school with his weighted blanket and a snack to feel calm and regulated. Maybe your daughter needs to jump on a trampoline for 20 minutes before she starts on her homework.
The key is that you get to know the child and what helps them keep regulated.
Giving them doses of sensory input throughout the day can keep their body and brain in that optimal thinking mode that we parents want them to be in! You might even try giving them this input every 2 hours since you are already going to be feeding and watering them then too! Right? Right?
Ok, but here comes our key to the game again….it’s not going to be enough for us to just say to our kids “go sit under your weighted blanket” or “go swing on the swings” or “go jump on the trampoline.”
Because with this, coregulation is needed again. We can certainly teach our children about their sensory needs or preferences and encourage them to seek out these tools independently—and hopefully this will be something they do as they get older so they can take the tools into adulthood with them.
BUT. Before a child can use these tools independently, they first need someone to help coregulate them with the tools.
“Let’s go sit under your weighted blanket together and read a book.”
“Let’s go outside for 10 minutes so you can show me your backflips on the trampoline before we make dinner.”
“Let’s go for a walk/bike ride together.”
When you model these behaviors and do them with your child, your child experiences the benefit of these sensory experiences to help regulate their bodies and you enjoy a moment of connection together-an experience that builds attachment! Win-win! We know this can be hard so check out the resources below for some tips and tricks!
If after reading through this you think, “I wonder if my child has a sensory processing issue?,” reach out to your County Director who can provide you with our sensory checklist as well as a resource we created to help families understand Sensory Processing Disorder more closely.
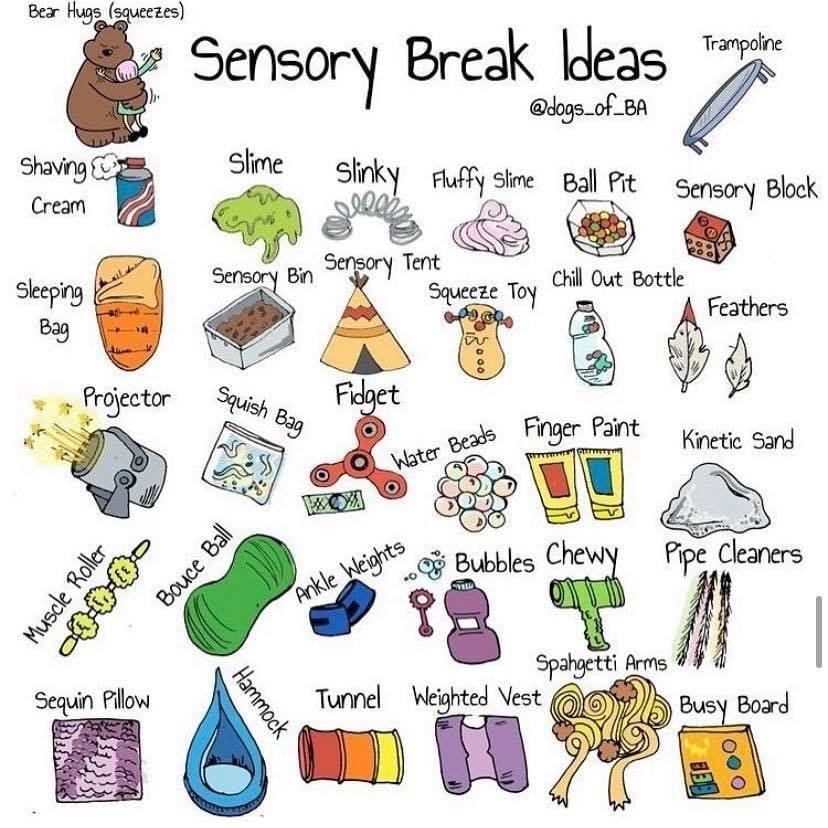
image from: https://childrenssensorytherapy.co.uk/
*A rich Sensory Diet is one of the Empowering Principles of Trust Based Relational Intervention (TBRI®). TBRI® is an attachment-based, trauma-informed intervention that is designed to meet the complex needs of vulnerable children. TBRI® uses Empowering Principles to address physical needs, Connecting Principles for attachment needs, and Correcting Principles to disarm fear-based behaviors. Learn more about TBRI® here: https://child.tcu.edu/